Updated August 16, 2021
Possibly the most frustrating disease of cats is stomatitis. It can cause terrible suffering, and for a third of affected cats, nothing seems to work well. For the other two thirds, the only good option is an extreme one.
New treatments have made the control of stomatitis within the reach of more cats, and we may be on the cusp of even greater things.
What Is Stomatitis?
Stomatitis, or more correctly gingivostomatitis, is inflammation of the mouth not directly associated with the teeth. The definition is important: many cats who are said to have stomatitis really have gingivitis and periodontitis. While still severe, these cats will respond to standard dental treatments and subsequent good oral hygiene.
Stomatitis on the other hand, is a poorly understood disease which likely represents malfunction of the immune system. It is said to affect anywhere between 0.7 and 12% of cats depending on how you define it.
The most common locations for stomatitis are at the back of the mouth at the opening to the throat (often called the fauces) and on the inside of the cheeks. Sometimes the tongue or oesophagus are also affected.
The Causes Of Stomatitis
Here is what we know about feline gingivostomatitis:
- Cats with stomatitis almost always also have regular tooth and gum disease, but not vice versa
- The risk of it developing goes up by 70% with each additional cat in the house (but removing them afterwards will not help)
- Affected cats are more likely to carry the calicivirus cat flu virus, and if they cure they will clear the virus
- The gums of affected cats contain more cytotoxic (killer) T cells than normal cats
- The risk increases with age
The best theory is that long-term immune stimulation in the mouth leads to the development of an abnormal, runaway immune response. This is certainly what I see: cats who develop stomatitis often have had more regular gum disease for years before it starts.
The Signs Of Stomatitis
Most of the signs of gingivostomatitis are due to severe pain. These include:
- Drooling, excess salivation and a dirty face
- Hissing or backing away during eating
- Extreme pain on opening the mouth
- Reluctance to eat hard food (though it is amazing how some cats will manage to keep eating)
Cats will also have a foul smell from the mouth, but this is true for all oral diseases. Diagnosis is usually straightforward but if the lesions are not symmetrical, a biopsy is a good idea to rule out cancers.
Treatment Of Stomatitis In Cats
Due to the slowly developing nature of the disease, most cats have tried some or all of the following by the time stomatitis develops:
- Regular dental cleaning
- Antibiotics
- Corticosteroids, especially prednisolone
These will all help to some extent, often quite well at the beginning but the effect reduces with time. Most cats end up needing a lot more treatment. The most important of these is pain control.
No matter what else we do, we need these cats to be comfortable, both for welfare reasons and so they look after themselves better. Drugs used are a combination of meloxicam, buprenorphine and gabapentin. In particular, buprenorphine (which is normally an injectable) works very well just by dripping it in the mouth.
However, even this is usually not enough.
Tooth Removal For Stomatitis
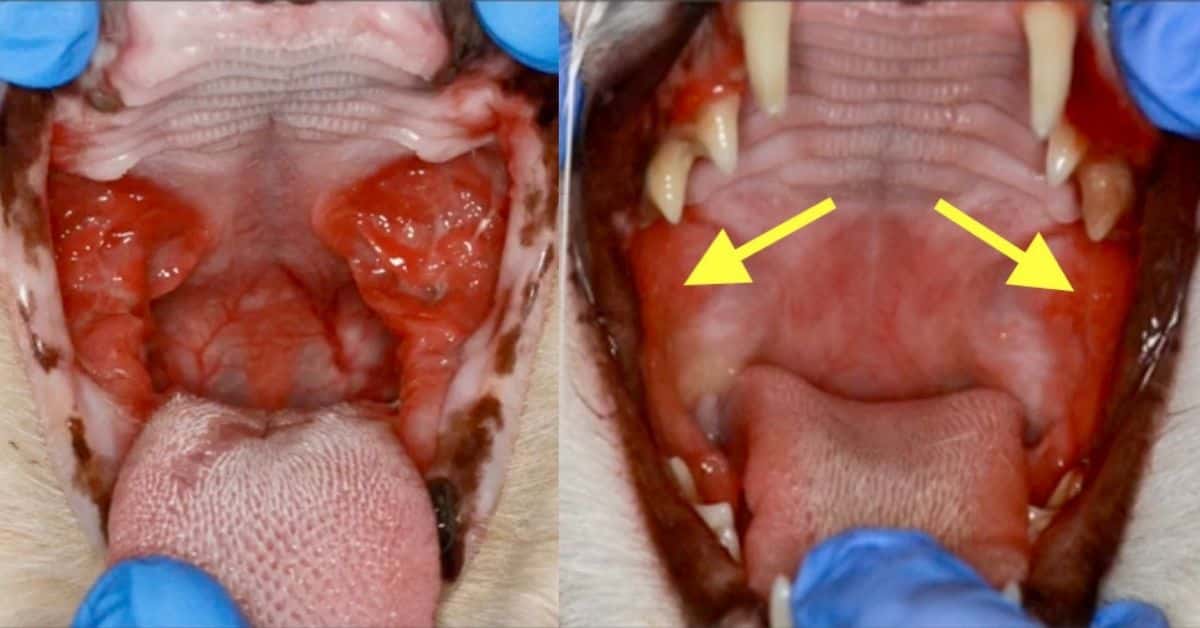
The best hope for a cat is that removal of their teeth will help. This is such a major hurdle to cat owners that I can spend six months trying to convince some to do it. But just look at these figures:
- 28.4% of cats are cured
- 39% are substantially improved
- 26.3% have minor improvement
- 6.3% do not respond at all
To the question of “how will they eat?” I answer that the pain is what is stopping them, not whether they have teeth or not. Commercial foods mean that cats don’t really need teeth anyway. All they need is to be happy.
Only the teeth at the back (premolars and molars) need removing in most cases. Leaving the canines and incisors means cats look and act much the same, and the procedure is shorter. However, at Walkerville we still often do only one side of the mouth at a time.
Close to 70% of cats who have their teeth removed will still need some form of medical treatment at least in the short term.
Newer Stomatitis Treatments
The real problem comes for the few cats who don’t respond to tooth extraction. If this happens to you, please don’t regret having the teeth removed; the next treatments are very unlikely to work on their own.
Cyclosporine is an immunosuppressant that helps in around a half of these cases, especially if blood levels are measured. Those that cure can usually be weaned off the drug, whereas others may need to stay on it for life. You can learn more about cyclosporine here.
Interferon Omega injections have a lower response rate (similar to prednisolone) but give a small chance of complete cure.
Mesenchymal Stem Cells given intravenously are the newest hope, and are showing good results in early trials. A seemingly effective product is close to release in the USA.
If no other treatments work, you should never feel guilty about choosing euthanasia. It’s a terrible choice, but also sometimes the only humane and kind thing for the worst of cases. But I hope I’ve helped you see that there’s a lot more than just cortisone and antibiotics, and a real chance of cure for many cats.
Have something to add? Comments (if open) will appear within 24 hours.
By Andrew Spanner BVSc(Hons) MVetStud, a vet in Adelaide, Australia. Meet his team here. The information provided here is not intended to be used as a substitute for going to the vet. If your pet is unwell, please seek veterinary attention.
References
Jennings, M. W., Lewis, J. R., Soltero-Rivera, M. M., Brown, D. C., & Reiter, A. M. (2015). Effect of tooth extraction on stomatitis in cats: 95 cases (2000–2013). Journal of the American Veterinary Medical Association, 246(6), 654-660
Lommer, M. J. (2013). Efficacy of cyclosporine for chronic, refractory stomatitis in cats: a randomized, placebo-controlled, double-blinded clinical study. Journal of veterinary dentistry, 30(1), 8-17

Is it at all possible that the following symptoms/diagnostics could indicate a somewhat probable indication of stomatitis? We recently had to put my 14 year old girl down and the entire time, though I know I am not a vet I only have a BS in Biology, I felt like the initial presentation was related to an issue in her mouth/esophagus. She was a very independent cat and the first sign we noticed was that she was plopping her paws in the water and we didn’t think she was drinking. Then she had the desire to eat(we offer both soft and kibble) b/c she’d go to the bowl and nearly ingest the food but something would stop her. She then started to lose weight. We took her to the vet and her bilirubin was very high, Liver enzymes were high, she had a UTI, great kidney function, and would not eat/drink urinate/defecate. We were told it was likely Liver Failure/Pancreatitis. She was treated with 3 days overnight stay with IV antibiotics, fluids, and Denamarin. When we took her home she seemed to improve for 2 days then crashed again. I noticed her chin must have been inflamed for some time b/c upon coming home(after having IV antibiotics) the size of her chin was noticeably smaller. I then noticed that 2 areas on her gums were seemingly inflamed; like 2 pea sized gum tissue. She had also previously came to love aggressively rubbing her chin against the comb we’d use to groom her. I just cannot help but think that the Liver and pancreas issues developed from an issue in her mouth; then I read this article and the description had struck a cord and was very inline with her presentation. That and a few other veterinary journal articles. At the time I hadn’t read as much about stomatitis as I have subsequently. Only looking for closure and to assure that my 16 year old cat won’t succumb to a similar issue. Thank you in advance.
Hi Matthew. I can assure are you that it is very unlikely the mouth was the cause of the problem. There are two reasons for this. Firstly, it is almost universal that owners of old unwell, cats believe the problem is with the mouth, due to the way the cats begin to play with or mouth their food instead of eating it. The true reason for this is probably a loss of appetite, combined with long-standing habits that make them continue to try. The second reason is that the disease described in this article is extremely obvious and impossible to miss. I’m sure your vets were on the right track, it’s just that nothing could be done.
Hi my little girl is having flares and we can’t get them under control as of yet. Is Interferon Omega available in the US?
Hi Michele. I think it is, but you’ll need to check with your local vet.
My little boy, whom I’ve had since he was about 3 weeks old, has stomatitis. He had his teeth removed, but to no avail. He’s had steroid shots the last three months, but the vet wants to space out the shots, though he shows signs of pain before a month is up. The vet has offered no other options. I am going to ask him about the ones mentioned above.
I think what I need to know is how I will know when it’s time to let him go. I don’t want him to suffer unduly.
Thank you so much.
Hi. If you are in touch with your cat’s feelings, and don’t try and hold onto them for your own sake, then you will just know. It’s extremely distressing to watch an animal in unrelenting pain and anyone with a clear mind does it easily.
Try Jarrow lactoferrin
1/2 capsule 2x daily mixed with canned food or all meat baby food.
Lactoferrin if found naturally in the mucous membranes of the mouth as well as in mothers milk( Colostrum)
I had to put my boy in the deep sleep a few days ago,I feel maybe the surgery went wrong even though they said it was successful,or I caused it by trying to feed him myself with a syringe,idk but I do know that I blame myself,I didn’t raise him from a baby,my father did,he told me he didn’t have a smelly breath until he got older,but never took him to the vet,I can’t stop thinking if I had taking him to the vet sooner I could have prevented him from being in pain,I was told that there was a fracture and there wasn’t anything they could attach wire to,so there was nothing they could do,I would have thought by now there would be other options, like plastic surgery or a to hold the jaw together so that he could use it again,just like we have available for humans,I didn’t give him he’s antibiotics that night either,I did try to get him to have some food or water though, I’m just not sure what went wrong but I do not he’s not with me anymore and hurts that I couldn’t do anything else for him we were so close.
Hi Kylie. It’s very unlikely that anything you did or did not do had any influence on this horrible disease. Do not blame yourself.
Can gabapentin be applied along the gum line like buprenorphine? My cat’s mouth is so inflamed, he does not want the meds shot into it now. Ditto prednisolone. He tolerates the buprenorphine on his gumline. Once the pain is under control again, we can resume syringe feeding hopefully today. He is having an unusually bad flare today.
Hi Casey. I have never heard of gabapentin being applied transmucosally and doubt it would work I’m sorry. I would be continuing with the buprenorphine.
i have had 4 cats with gingerstomiatis sadly ruby was put to sleep in june broke my heart
i have brother who also has this but not as bad he has the ulcers on his thorat hes on loxicom
i have another cat bruce hes in a very bad way and i know the vet wants him put to sleep hes fed via towel blended food 3 times a day hes tiny and thin he had server stomaitiis and many ulcers his mouth red raw he also has cat flu too
i love him
one of his daughters has stomotoits too she had teeth out like her dad ahd shes doing ok
ive but him in a steamer to help hi breath what else can i do
i love them sooo much
Hi Jayne. I’m sorry to hear about that. I don’t have any additional advice other than what is contained in the article. Good luck.
Oh my goodness. reading this breaks my heart. I have 3 my own bud one of them a boy Jackson has the virus on his gums and I had been told by a vet today, about the teeth removal et c. I am so so sorry and wish there would b a cure.
Hello,
I adopted my 7 year old cat 5 months ago and he was diagnosed with stomatitis. I do not know how long he has had this. Will he die?? I have an surgery scheduled for him in November.
Hi Jessica. You’ll find the best answers I can give to your question in the article above.
I am so sad to say that my baby British Shorthair male cat (5 years old neutered) has had this from baby age when the vet said ‘oh i feel so sorry, gums are red, such sadness’ and i had no clue what she is talking about. My cat been on abntibiotics, anti inflamatory, or the pain killers, he had a fall out with his other bshs who had to find a new home because of such cat conflict and never worked out when we re introduced them. To cut the story (that would be a book to write) my cat suffers most times. Back of his two gums have been taken off. And he’s been on antibiotics many times and b complex injection for immune system. What else would you recommend? his front gums are clean, but when he was stressed there were many ulcers which 1 month antibiotics helped. But recently he is back on stinking breath. I feel so sorry for him. I feed him grain free wet food, and have to hand feed him because he is fussy eater and that, we are not sure whether anything from the mouth or personality. He’s had blood tests as well all types. I wish you could find something to give me hope, and yes, maybe taking all the gums isn’t a good idea, this thing will still pop over and over. How long do they live? Please give me hope. Thank you. x
Hi Donita. My recommendations can be found in the article. Good luck.
This is so very painful for the cats. Please have a talk with him, tell him what a great baby he’s been and how much he filled a space in your life, and how much you love him and will miss him always, but you will be reunited one day, then let him go. Would you want to be force fed, medicated and in pain all the time? The poor babies starve to death. I’m saying this because I just lost one over Thanksgiving weekend, unable to get to her to her regular vet and was only able to see an alternative vet for a strong antibiotic shot. She died 3 days later during the night. It was horrible to watch her starve to death. I tried to get her in to have her put to sleep, but she died before they could euthanize her. I’m facing this same thing with my 14 year old diabetic cat now. He has severe ulcerations from stomatitis and all the can do is give him pain meds, steroids and try to make him comfortable. This breaks my heart, but I will give it a try and see if he’ll be able to eat. If he doesn’t get better, I’ll have to have that talk with him, too. So very sorry. God bless you and kitty. Pam
My cat has terrible breath and I think he’s got gingivitis, can human gabapiton help with his pain?
Hi Cathy. The only solution for a cat with oral pain is to see a vet and get it treated properly. Please do not give medications like these without communicating with your local vet first. It’s likely to do more harm than good.